In the realm of healthcare, the judicious use of antibiotics has become an increasingly critical issue, particularly in the treatment of upper respiratory infections (URIs) by a Family Doctor. These common ailments, encompassing a spectrum of viral and bacterial infections affecting the nose, throat, and sinuses, are a frequent cause of visits to walk-in and Family Doctor’s clinics . However, the indiscriminate use of antibiotics in URI management has raised concerns regarding antibiotic resistance, adverse effects, and the overall efficacy of treatment strategies. This underscores the importance of antibiotic stewardship—a concerted effort to optimize antibiotic use while minimizing unnecessary prescribing.
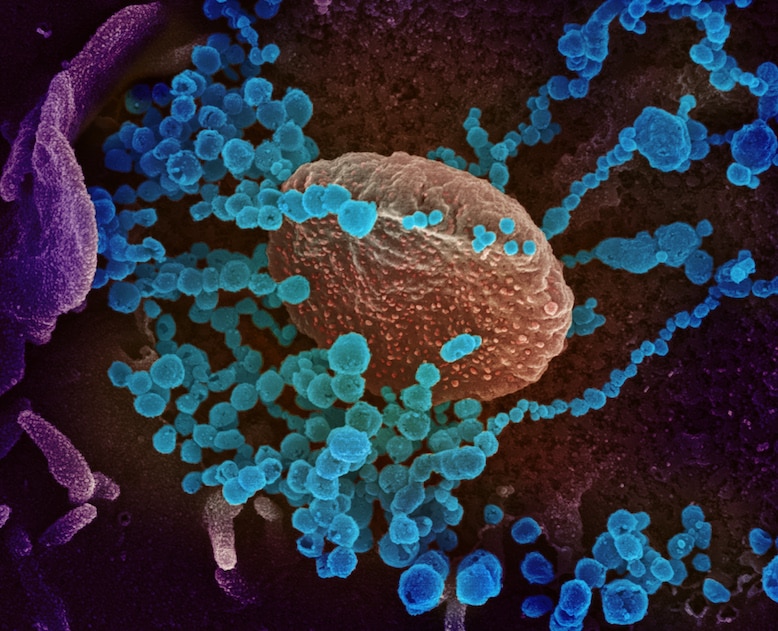
Upper respiratory infections, often referred to as the common cold, are predominantly viral in nature. Rhinovirus, coronavirus, adenovirus, and respiratory syncytial virus (RSV) are among the most common viral culprits responsible for these infections. While antibiotics are effective against bacterial URIs, such as those caused by Streptococcus pneumoniae or Haemophilus influenzae, they hold little to no benefit in treating viral URIs. Yet, despite this distinction, antibiotics continue to be prescribed at alarming rates for URI management, contributing to the global burden of antibiotic resistance.
The consequences of antibiotic overuse are far-reaching and multifaceted in Family Medicine. Antibiotic resistance—the ability of bacteria to withstand the effects of antibiotics—poses a significant threat to public health, rendering once-effective treatments ineffective and limiting options for future infections. Furthermore, indiscriminate antibiotic use disrupts the delicate balance of microbial communities in the body, leading to adverse effects such as gastrointestinal disturbances and increased susceptibility to opportunistic infections.
To address these challenges, antibiotic stewardship programs have emerged as a cornerstone of Family Doctor’s efforts to promote responsible antibiotic use. These programs aim to optimize antibiotic prescribing practices through a combination of education, guidelines, and surveillance. In the context of URIs, antibiotic stewardship emphasizes the following principles:
- Diagnostic Precision: Accurate diagnosis is paramount in guiding appropriate treatment decisions for URIs. Healthcare providers must differentiate between viral and bacterial infections through clinical evaluation and, when necessary, diagnostic testing. Rapid antigen tests and culture-based methods can help identify bacterial pathogens, informing targeted antibiotic therapy when warranted.
- Evidence-Based Prescribing: Antibiotic prescribing should align with evidence-based guidelines and recommendations tailored to the specific etiology and severity of the infection. For viral URIs, supportive care strategies—including rest, hydration, and symptom relief with over-the-counter medications—are the mainstay of treatment. Antibiotics should be reserved for bacterial URIs and cases where complications or bacterial co-infections are suspected.
- Patient Education: Empowering patients with knowledge about the nature of URIs and the appropriate use of antibiotics is essential in fostering shared decision-making and adherence to treatment plans between patients and their Family Doctor. Educating patients about the self-limiting nature of viral infections, the ineffectiveness of antibiotics against viruses, and the importance of completing prescribed courses of antibiotics for bacterial infections can help mitigate unnecessary antibiotic use.
- Monitoring and Feedback: Ongoing monitoring of antibiotic prescribing practices and patient outcomes allows healthcare institutions to evaluate the impact of antibiotic stewardship initiatives and identify areas for improvement. Feedback mechanisms, coupled with regular review of prescribing patterns and antibiotic resistance data, facilitate continuous quality improvement efforts.
- Collaborative Approach: Antibiotic stewardship requires collaboration across healthcare disciplines, including walk-in clinics, Family Medicine physicians, pharmacists, and infection control specialists. Multidisciplinary teams can work together to implement best practices, promote antimicrobial stewardship awareness, and foster a culture of responsible antibiotic use within healthcare settings.
Antibiotic stewardship plays a pivotal role in navigating the complexities of URI management, balancing the need for effective treatment with the imperative to safeguard the long-term efficacy of antibiotics. By embracing the principles of diagnostic precision, evidence-based prescribing, patient education, monitoring, and collaboration, healthcare providers can optimize antibiotic use, preserve antibiotic effectiveness, and promote patient-centered care in the era of antibiotic resistance. Together, we can chart a course towards a future where antibiotics remain a cornerstone of modern medicine, serving as invaluable tools in the fight against infectious diseases.


Leave a Reply